
CMS released the final 2021 Physician Fee Schedule (PFS) along with several interim final rules. Review a breakdown of key payment and policy updates.
Key insights
- CMS moves forward with 2021 E/M changes with impacts to both RVU levels and payment rates for all CPT codes.
- Telehealth and virtual health have been expanded.
- We can help you review this long and daunting set of new changes.
Looking for guidance on the CMS payment rules?
On December 1, 2020, the Centers for Medicare & Medicaid Services (CMS) released the final 2021 Physician Fee Schedule (PFS) along with several interim final rules. This regulatory advisor will cover some of the key changes, but not everything in the rule. Download the final rule (CMS-1734-F) from the Federal Register to review in full.
CLA can help
Are you aware of the E/M code and Relative Value Unit (RVU) changes in 2021? Did you know they may have implications for your practice’s operations, revenues, compensation structure, and more? We can explain how and why, to help you create your path forward. Reach out today for assistance.
Key payment updates
Evaluation and Management (E/M)
As a reminder, CMS finalized various changes to office/outpatient (O/O) E/M services visit code set (99201–99215) in the 2020 PFS rule, effective January 1, 2021. Those include a new documentation framework where the history and exam are no longer used to select the code level for O/O E/M visits, but rather uses total time or level of medical decision making (MDM). The history and exam components will only be performed when (and to the extent) reasonable and necessary, and clinically appropriate.
CMS deletes 99201 (Level 1 O/O visit, new patient). Levels 2 through 5 O/O E/M visits are based on MDM or the total time personally spent by the reporting practitioner on the day of the visit (including face-to-face and non-face-to-face time). CMS finalizes a new prolonged visit add-on code with payment under G2212 and discontinued use of 99358 and 99359 (prolonged E/M visit without direct patient contact). CMS also finalizes separate payment for G2211 to provide payment for visit complexity inherent to E/M associated with medical services.
The code set was resurveyed and revalued, after which CMS adopted new values for 99202–99215 and assigned Relative Value Units (RVUs) to the new E/M prolonged visit code G2212, as well as the new code G2211. These are effective January 1, 2021.
Conversion factor, estimated impact
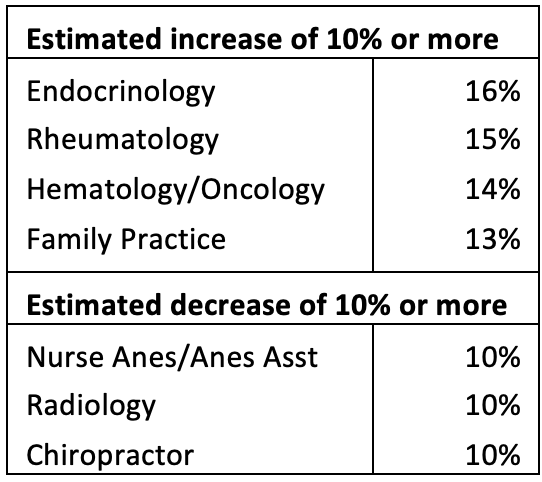
The E/M changes and revalued RVUs have budget neutrality implications. To maintain budget neutrality, CMS sets the conversion factor at 32.4085, a decrease from last year of 10.2%. When the E/M code set, RVU changes, and the conversion factor are combined, the impact by specialty varies. CMS provides an estimate of these impacts in Table 106 in the final rule. The chart (at right) shows impacts (positive or negative) at or above 10% by service type.
Due to these estimated impacts, some health care stakeholder groups reached out to Congress to intercede. Congress partially mitigated these cuts under the Consolidated Appropriations Act, 2021 (CAA, 2021), enacted December 27, 2020.
Consolidated Appropriations Act, 2021
The law includes one-time funding to partially offset PFS budget neutrality concerns for 2021. By doing so, the payment reduction is decreased to 3.32% instead of the previous 10.2%. CMS subsequently released an updated conversion factor of 34.8931. Notably, the increased funding applies only to 2021. In addition, the law stops CMS from paying for G2211 (or any successor or substantially similar code) prior to January 1, 2024. Review CLA’s coverage of the health care policies in the CAA, 2021.
Refinements and revaluing
CMS makes many other changes to codes which are too numerous to include in this regulatory advisor. Some examples include RVU updates for following codes sets:
- End-stage renal disease monthly capitation payments
- Transitional care management
- Maternity services
- Assessment and care planning for patients with cognitive impairment
- Initial preventive physical examination
- Initial and subsequent annual wellness visits
- Emergency department visits
- Therapy evaluations
- Behavioral health care services
CMS also reviews and addresses other new, revised, or potentially misvalued codes.
Principal Care Management (PCM) in Federally Qualified Health Centers (FQHCs) and Rural Health Clinics (RHCs)
CMS finalizes the addition of G2064 and G2065 to G0511 as a comprehensive care management service for RHCs and FQHCs starting January 1, 2021. The two codes will be used in calculating the average of the national non-facility PFS payment rates for G0511. RHCs and FQHCs will be able to bill for PCM services using G0511, either alone or with other payable services on an RHC or FQHC claim.
FQHC market basket
CMS finalizes the 2021 productivity-adjusted FQHC market basket update as 1.7%. This reflects a 2.4% increase in the proposed 2017-based FQHC market basket and a 0.7% adjustment for productivity.
Key policy updates
Telehealth
CMS finalizes a variety of changes to its telehealth policies:
- Permanent addition of codes (Category 1) — CMS finalizes nine additions to the telehealth list under Category 1:
- Group psychotherapy (90853)
- Neurobehavioral status exam (96121)
- Domiciliary, rest home or custodial care, established patients (99334-99335)
- Home visits, established patients (99347-99348)
- Cognitive assessment and care planning services (99483)
- Visit complexity inherent to certain office/outpatient E/M (G2211)
- Prolonged office/other outpatient E/M services (G2212)
- Temporary addition of codes (Category 3) — CMS finalizes its new category, Category 3, for codes to remain on the telehealth list temporarily. CMS indicates the temporary codes will be allowed through the end of the year in which the public health emergency (PHE) ends or December 31, 2021. CMS had originally proposed 13 codes under Category 3 but finalized the inclusion of 63 codes for the list:
- End-stage renal disease monthly capitation payment services (90952–90953, 90956, 90959, 90962)
- Emergency department visits (99281–99285)
- Domiciliary, rest home or custodial care, established patients (99336–99337).
- Home visits, establish patients (99349–99350)
- Nursing facilities discharge day management (99315–99316)
- Psychological and neuropsychological testing (96121, 96130–96133, 96136–96139)
- Therapy services, physical and occupational therapy, all levels (97161–97168, 97110, 97112, 97116, 97535, 97750, 97755, 97760–97761, 92521–92524, 92507)
- Subsequent observation and observations discharge day management (99217, 99224–99226)
- Initial hospital care and hospital discharge day management (99221–99223, 99238–99239)
- Critical Care Services (99291–99292)
- Inpatient neonatal and pediatrics critical care, subsequent (99469, 99472, 99476)
- Continuing neonatal intensive care service (99478–99480)
- Frequency limits — CMS finalizes that the frequency limitation for subsequent nursing facility visits is one Medicare telehealth visit every 14 days in the nursing facility setting.
Communication Technology Based Services (CTBS)
- For HCPCS G2061–G2063, CMS finalizes permanently extending the ability for clinical social workers and clinical psychologists, as well as physical therapists (PTs), occupational therapists (OTs), and speech language pathologists (SLPs) who bill Medicare directly for their services (when the service furnished falls within the scope of these practitioner’s benefit categories) to bill for these services. These flexibilities were provided during the PHE and are now permanent.
- CMS finalizes two additional G codes for certain nonphysician practitioners (NPP) who cannot independently bill for E/M services:
- G2250 — Remote assessment of recorded video and/or images submitted by an established patient (e.g., store and forward) including interpretation with follow-up of the patient within 24 business hours, not originating from a related service provided within the previous seven days nor leading to a service or procedure within the next 24 hours or soonest available appointment.
- G2251 — Brief communication technology-based service (e.g., virtual check-in) by a qualified health care professional who cannot report E/M services, provided to an established patient, not originating from a related service provided within the previous 7 days nor leading to a service or procedure within the next 24 hours or soonest available appointment; 5–10 minutes of medical discussion.
- CMS finalizes valuing these services identically to G2010 and G2012, respectively.
- CMS finalizes designating these codes and G2061–G2063 as ‘‘sometimes therapy’’ services.
- On an interim basis through 2021, CMS finalizes an extended audio-only assessment service. This is not considered “telehealth” but rather CTBS. Billing for the code will mirror G2012.
- G2252 — Brief communication technology-based service (e.g., virtual check-in) by a physician or other qualified health care professional who can report E/M services, provided to an established patient, not originating from a related E/M service provided within the previous seven days nor leading to an E/M service or procedure within the next 24 hours or soonest available appointment; 11–20 minutes of medical discussion.
Remote Physiologic Monitoring (RPM)
For CY 2021, CMS provides clarifications on how it reads code descriptors and instructions associated with 99453, 99454, 99091, 99457, and 99458.
On January 11, 2021, CMS released technical corrections to the final 2021 PFS rule.
CMS clarifies that for 99453 and 99454, they are to be reported only once during a 30-day period even if multiple medical devices are provided to a patient. Additionally, CMS reiterates that services associated with all the medical devices can be billed by only one practitioner, only once per patient, per 30-day period, and only when at least 16 days of data have been collected, and that the services must be reasonable and necessary. CMS also reminds providers to use and bill a more specific code if available. For example, 95250 would be used for continuous glucose monitoring.
- CMS states that the RPM process begins with 99453 and 99454, both practice expense (PE) codes only. As PE-only codes, they are valued to include clinical staff time, supplies, and equipment, including the medical device for the typical case of remote monitoring.
- CPT code 99453 (remote monitoring of physiologic parameter(s), e.g., weight, blood pressure, pulse oximetry, respiratory flow rate, initial; set-up and patient education on use of equipment) is valued to reflect clinical staff time that includes instructing a patient and/or caregiver about using one or more medical devices. CMS notes it may only be billed once per episode of care. Under the CPT Codebook, an episode of care begins “when the remote physiologic monitoring service is initiated and ends with attainment of targeted treatment."
- CPT code 99454 (remote monitoring of physiologic parameter(s), e.g., weight, blood pressure, pulse oximetry, respiratory flow rate, initial; device(s) supply with daily recording(s) or programmed alert(s) transmission, each 30 days) is valued to include the medical device or devices supplied to the patient and the programming of the medical device for repeated monitoring. CMS clarified the PE inputs for 99454; the medical devices that are supplied to the patient and used to collect physiologic data are considered equipment and, as such, are direct PE inputs for the code.
- CMS states that after analyzing and interpreting a patient’s remotely collected physiologic data, next in the RPM process is the development of a treatment plan that is informed by the analysis and interpretation of the patient’s data. At this point, the physician or NPP develops a treatment plan with the patient and/or caregiver (that is, develops a patient-centered plan of care) and then manages the plan until the targeted goals of the treatment plan are attained, which signals the end of the episode of care. The codes are:
On January 11, 2021, CMS released technical corrections to the final 2021 PFS rule
CMS clarifies that the 20-minutes of intra-service work associated with 99457 and 99458 includes a practitioner’s time engaged in “interactive communication” as well as time engaged in non-face-to-face care management services during a calendar month.
- 99457 (remote physiologic monitoring treatment management services, clinical staff/physician/other qualified health care professional time in a calendar month requiring interactive communication with the patient/ caregiver during the month; first 20 minutes).
- 99458 (remote physiologic monitoring treatment management services, clinical staff/physician/other qualified health care professional time in a calendar month requiring interactive communication with the patient/caregiver during the month; each additional 20 minutes listed separately in addition to code for primary procedure)
- Both codes describe the treatment and management services associated with RPM. CMS indicates stakeholders requested additional clarification on various aspects of these codes, primarily, who can furnish the codes as well as wanting details on “interactive communication” with a patient. CMS responds that it addressed who can furnish 99457 and 99458 in the Calendar Year 2020 PFS final rule (84 FR 62697–62698) when they designated both codes as care management services. CMS explained that, like other care management services, those may be furnished by clinical staff under the general supervision of the physician or NPP. CMS also clarified that ‘‘interactive communication’’ for purposes of 99457 and 99458 involves, at a minimum, a real-time synchronous, two-way audio interaction that is capable of being enhanced with video or other kinds of data transmission.
- CMS highlights that regardless of the number of medical devices, the services for all the devices can only be billed once per patient per 30-day period and only when at least 16 days of data has been collected.
- CMS clarifies that as E/M codes, CPT codes 99453, 99454, 99091, 99457, and 99458, can be ordered and billed only by physicians or NPPs who are eligible to bill Medicare for E/M services.
- Data should digitally (that is, automatically) upload patient physiologic data (that is, data are not patient self-recorded and/or self-reported).
- CMS clarifies that the medical device needs to meet the FDA’s definition of such a device but does not need to be FDA approved.
- RPM services may be used with patients with chronic conditions and, going forward, may be used with acute conditions.
- CMS permanently finalizes on a permanent basis, the rule allowing consent to be obtained at the time that RPM services are furnished, and allowing auxiliary personnel (which includes other individuals who are not clinical staff but are employees or leased or contracted employees) to furnish services described by CPT codes 99453 and 99454 under the general supervision of the billing physician or practitioner.
Transitional Care Management (TCM)
CMS finalizes the removal of 14 additional actively priced (not bundled or noncovered) codes related to end-stage renal disease services from the list of codes that cannot be billed concurrently with TCM. Additionally, CMS finalizes their proposal on G2058 related to Chronic Care Management (which CMS finalizes in this rule as new 99439). As such all 15 codes may now be billed concurrently with TCM when reasonable and necessary.
Psychiatric Collaborative Care Model (CoCM) Services
CMS finalizes its proposal related to G2214:
- G2214 — Initial or subsequent psychiatric collaborative care management, first 30 minutes in a month of behavioral health care manager activities, in consultation with a psychiatric consultant, and directed by the treating physician or other qualified health care professional.
- Valuation of G2214 is based on one half of the time described by the existing code, 99493. As such, the RVU for the new code is 0.77.
- G2214 may be used for either the initial month or subsequent months.
- CMS indicates the required elements listed for 99493 would also be required elements for billing for G2214 and CPT time rules would apply, consistent with the guidance in the CPT codebook for CPT codes 99492–99494. In addition, general supervision applies.
Supervision rules
CMS finalizes various flexibilities related to Medicare supervision rules:
- Teaching physician/resident supervision flexibilities — CMS provided flexibility during the PHE related to physician supervision requirements with residents. In general, CMS extends these flexibilities through the end of the PHE but will not make them permanent. However, CMS did finalize several changes permanently:
- A permanent policy to permit teaching physicians to meet the requirements to bill for their services involving residents through virtual presence, but only for services furnished in residency training sites that are located outside of an Office of Management & Budget defined Metropolitan Statistical Area (MSA).
- A permanent policy that relates to Medicare telehealth and allows payment for teaching physicians when a resident furnishes Medicare telehealth services in a residency training located outside of a MSA to a beneficiary who is in a separate location outside the same MSA as the residency training site, or is within a rural area outside of a different MSA, while a teaching physician is present through interactive, audio/video real-time communications technology (excluding audio-only), in a third location, either within the same rural training site as the resident or outside of that rural training site.
- A permanent policy for residency training sites located outside of an MSA. The policy allows Medicare payments to the teaching physician when the resident furnishes an expanded list of services under the primary care exception. These will include CTBS and interpersonal consults (99421–99423 and 99452, G2010, G2012), but will not include E/M services with moderate to high complexity or TCM services (CPT codes 99204, 99214, 99205, 992215, 99495 and 99496). The latter will be removed from the primary care exceptions list at the end of the PHE.
- Diagnostic testing — CMS finalizes its proposal allow nurse practitioners, clinical nurse specialists, physician assistants (PAs), and clinical nurse midwives to supervise certain diagnostic tests consistent with state law and scope of practice requirements. For PAs, CMS indicates there is not a specified supervision level of supervision assigned to individual tests.
- Maintenance therapy — CMS makes permanent beginning January 1, 2021, a policy that allows PTs or OTs who established a maintenance program to assign the duties to a physical therapy assistant or occupational therapy assistant, as clinically appropriate, to perform maintenance therapy services.
Medicare Shared Savings Program (MSSP)
CMS makes a series of changes to the MSSP, several of which are to:
- Modify quality performance measurement.
- Change the methodology for determining shared savings and shared losses based on Accountable Care Organizations (ACO) quality performance.
- Revise the approach to monitoring ACO quality performance and addressing ACOs that fail to meet the Quality Performance Standard.
- Update the process used to validate ACO Quality Data Reporting.
- Update the extreme and uncontrollable circumstances policy as it relates to quality performance.
- Update the definition of primary care services used in beneficiary assignment and codify in regulations the adjustment that is made to an ACO’s historical benchmark to reflect any changes to the beneficiary assignment methodology during an ACO’s agreement period.
- Revise the repayment mechanism arrangement policy.
How we can help
Connect with CLA for further clarification on the final rule and how these payment and policy changes may impact your organization. Our team of health care professionals are here to help.
